Hi everyone,
I've moved this blog onto www.iwanttobeasurgeon.com which I have also given a little makeover! Hope you like it and let me know what you think...
Amel
Saturday, 10 March 2012
Thursday, 9 February 2012
February Journal Club
Firstly, congrats to everyone who has finished CST interviews. Its not to much longer before you find out the good news (fingers crossed). Anyway, I have decided to choose a systematic review on Negative pressure wound therapy ("Vac dressings") for this month's journal club. I find this subject incredibly interesting and have been working on a review of my own after being inspired by Dr Paul Liu who was the Chief of Plastics at Rhode Island Hospital where I did my placement last summer. As always, the article details are below and I will put up my comments in the next few days. I would be interested in what every one else thinks.
J Plast Reconstr Aesthet Surg. 2012 Jan 9. [Epub ahead of print]
The methodology of negative pressure wound therapy: Separating fact from fiction.
Labels:
Basic surgical skills,
Education,
Pathology,
research,
Surgery
Tuesday, 17 January 2012
Core Surgery Applications - Part II The Interview
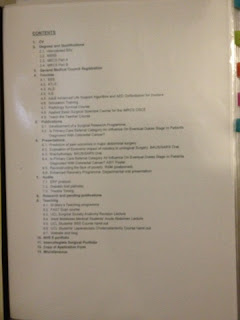
a) The hard portfolio
b) The actual interview
The hard portfolio is a very important way to demonstrate all your skills, achievements and also your organisation. Its upto you whether you use a lever arch file with dividers or a book. Either way there are principles that you must follow and some tips to make your book look impressive:
- Have a contents page and ensure dividers correspond with this
- Organise your book in logical sections
- Avoid bunching up lots of pages in one pocket, your portfolio should read like a book so that interviewers can quickly flick through
- Include a recent copy of your CV after the contents
- Ensure that you add any certificates for courses as well as your MBBS certificate etc...
- Don't forget your GMC certificate, copy of your application form and anything else they mention on the website
- Organise printouts from your e-portfolio into CEXs in one pocket, dops in one pocket etc with the most recent and flattering first! Also don't forget the minipats/msf print outs
- If you can print copies of presentations/posters in colour then please do to make them stand out
- Don't forget teaching achievements!!!
- If you have a record of the operations you have helped in/done so far that will also be impressive. As a non trainee you can register and use the Intercollegiate Surgical curriculum Portfolio "ISCP" (www.iscp.ac.uk). I recommend this as it shows that you are already familiar with the programme that they will use for all surgical training. It is also a very nice way to display your operative rcord (if you have one). Do not worry about absolute number of surgeries as they know that not everyone has had much exposure to surgery.
- Be comfortable and prepared to reply to any question on anything in your portfolio!!
I have included pictures of my portfolio below to give you an example of how you can set one out if you're not sure where to begin.
The next bit is the actual interview. There are many books to help you prepare, the one I recommend is "
Medical Interviews: a comprehensive guide to CT, ST and Registrar interview skills - Over 120 medical interview questions, techniques and NHS topics explained". It has lots of good examples and basically goes through how to structure answers to questions. Also, this WEBSITE has some good free content.
First of all, turn up looking smart and clean as well as early. Make sure you have brought your portfolio as well as all the necessary paperwork including photocopy of front cover of your passport, photo ID, passport pics etc... Try not have a smoke (or drink) before hand ;)
My interview (in 2011 for the London Deanery at Lions court) was split into three sections:
CLINICAL STATION:
please note. This is the most important station and weighted the most. I had two examiners and each gave me a scenario to answer.
- The first scenario was of an elderly woman post anterior resection 1 day ago. You are called to see her as she has a low urine output. It is important with this question to say you would firstly ensure that basic ALS principles are applied by ensuring patient was stable ie ABC... Then I said I would take a history and examine the patient to look for evidence of bleeding, infection, peritonism (think anastomotic leak) etc... Then look at the obs chart and look at trends for urine, fluid balance, BP, PR, temperature as well as latest bloods esp post-op. I would ensure patient is stable and let registrar and consultant know. You need to mention what possible differentials are going through your head and how you would exclude...
- The second Scenario was of a patient who rolled over in bed and came to A+E with a fractured humerus. BE ACREFUL AND LISTEN TO QUESTION AS I APPROACHED THIS AS A TRAUMA AS THOUGHT HE FELL BUT ITS NOT! Basically, on xray he ad luscent areas. You need to say you would suspect pathological fracture and screen for malignancy through history, exam and then can possibly send off tumour markers/myeloma screen etc... make sure you show them you know which tumours metastasise to bone and how you would check for them.
- Some of my friends got asked how they would manage a kid who came in with a supraconduylar fracture (must talk about risk of neurovascular compromise if displaced) as well as abdominal tenderness after falling off tree. In both these scenarios ATLS principles are important and ensuring you tell seniors early on (the latter point goes for everything)
MANAGEMENT STATION:
This station was a tad disorganised. I was again given two scenarios to talk through.
- The first was that one of my F1's tells me that he felt persecuted by the Consultant. You have to show that you would be understanding and caring toward your colleague but also resepctful of the right channels to pursue. You would ask them why they feel bullied. If its because they don't have enough knowledge maybe you could offer to tutor them etc. Otherwise you would encourage them to discuss with their supervisor/pastoral mentor to get advise. You would act in a supporting role. Whatever you do, don't say you would tell them to "man up" - it doesn't go down well no matter how tempting...
- The next was how would I ago about organising the rota - snooze fest! Basically you need to balance adequate training in terms of clinic, study leave, operating time with annual leave. I spent a lot of time talking about annual leave, THEY WERE NOT IMPRESSED!! Basically rota also needs to be EWTD compliant so other ways you can ensure people get adequate training is by using simulators etc...
PORTFOLIO STATION:
By far, this was the nicest station although it is less weighted than the others. I had a panel of 4 judges and they had looked through my portfolio before-hand (you hand it in before your other stations start) and asked questions about my teaching (including plans I had for developing this blog and website :)). I was also asked:
- What speciality I want to do and why? (I mentioned plastics and also let them know that I am aware how competitive it is by rattling off some statistics on past numbers etc)
- How will I develop my CV to increase my chances of getting a number in plastics?
- Other people where asked: what in their CV shows a dedication and commitment to medicine, teaching, why they chose that particular deanery...
Anyway, I hope some of this is useful and I will try and get some more info on his year's interviews to help next year's applicants. Good luck and remmebr to be confident, relaxed and know your porfolio/CV.
Friday, 9 December 2011
Core Surgery Applications - Part I (the form)
So, most people will be finishing off their forms by now and I thought I'd thrown in a few last minute tips on completing your applications.
1) Firstly, brevity is essential! Most of the questions are limited to 65 words!! Ensure every word counts but write in clear and concise sentences. Bullet points look scruffy and unprofessional. You do not have space to list every achievement so highlight the most impressive and quickly mention the others.
2) Be honest. Whilst its important to "big up" your achievements, lying will only hurt your chances at interview as they can be very thorough with questioning. Also this is a probity issue and can lead to referral to the GMC.
3) Teaching is a very important part of being a surgeon. Don't just list your teaching experiences. If you have organised teaching then explain this, mention any feedback you have received and any plans you have to build on your experiences. Also, if you have had any training or attended a course to help with teaching then also state this.
4) Audits. Be honest and explain how you contributed to each audit. Also, whether outcomes were implemented and if re-audit has been done (state this as that's key to finishing the audit loop). If the audit has been presented or published then state this too. If you have done tons of audits then state how many and highlight a few examples rather than listing everything.
5) Commitment to speciality. This is very personal and I think you need to show how long you have been interested in the speciality and how you have explored it further. Mention electives, courses, placements, research, if you have sat any exams etc...
Anyway, I know this is brief but just wanted to give a few ideas out there. Please note, I am only posting my opinion but I do not know what the Deaneries are looking for and how they mark these questions. This is just advise based on experience of having applied last year and as such should not be taken as anything more than this. I do not accept any liability for any unsuccessful applications (sorry).
Good luck!!!
Amel
Thursday, 10 November 2011
Hand Surgery and so much more!
For anyone interested in hand surgery and/or working in developing countries and/or anatomy and/or art:
www.donaldsammut.com
I went to a talk he gave at the RSM on tuesday and it left me very impressed and inspired. In fact the whole evening was a great start to the Plastics section.
www.donaldsammut.com
I went to a talk he gave at the RSM on tuesday and it left me very impressed and inspired. In fact the whole evening was a great start to the Plastics section.
Journal Club - November
Hi all,
I was very impressed by the response to the first journal club paper. This month, I have chosen a paper that is very clinically relevant and addresses a common problem but management is often fraught with controversy. So this month's paper is:
I will pot my assessment in a few days time and would appreciate any input from you guys. Also if you would like to suggest any papers for next month, please go ahead! I would welcome input. FINALLY, I shall be putting up some posts on core training applications soon as well as more MRCS advice...
I was very impressed by the response to the first journal club paper. This month, I have chosen a paper that is very clinically relevant and addresses a common problem but management is often fraught with controversy. So this month's paper is:
J Bone Joint Surg Br. 2011 Oct;93(10):1362-6.
The non-operative functional management of patients with a rupture of the tendo Achillis leads to low rates of re-rupture.
I will pot my assessment in a few days time and would appreciate any input from you guys. Also if you would like to suggest any papers for next month, please go ahead! I would welcome input. FINALLY, I shall be putting up some posts on core training applications soon as well as more MRCS advice...
Labels:
Education,
exams,
Jobs,
Journal Club,
orthopaedics,
Teaching,
Training
Friday, 9 September 2011
MRCS Part B - Stations from yester year
Now please note, these stations are just to help give you an idea of what kind of topics could come up in the exam. There is no guarantee that they will come up again or even if they do the format maybe different as the exam structure has recently changed. MRCS OSCEs are designed to test your core surgical knowledge and ability. If you revise the theoretical stuff and ensure that you get experience in going to a variety of outpatient clinics as well as scrubbing in regularly in the OR then you should not have any problems.
Hope these are useful and good luck!
Clinical Skills and History Taking
1. Examine this ladies neck I started peripherally with a thyroid status exam, but the examiner prompted me to go directly to the neck. She was an afrocarribean lady with what I thought was bilateral parotid enlargement:
Q's
• Causes of symmetrical bilateral parotid enlargement
• What is most likely cause in her (sarcoidosis)
• He asked me about other manifestations outside the neck
2. Examine this lump on a man's back:
Large lipoma- I examined including assessing for fixity to muscle, transillumenence, draining lymph nodes etc
Q's
• What muscle was it overlying
• What is blood supply and lymph drainage of that muscle (was Lat Dorsi)
• To describe how you would excise this lipoma
• Consent patient for procedure
3. HISTORY:
Very simple history for likely colorectal Ca,
Q's
• RF for colorectal ca
• Difference in presentation for IBD and colorectal ca --> why is this change in bowel habit Crohns or UC
• How you would investigate him
• Why CT pneumocolon is inferior to colonoscopy (you can biopsy with latter)
4. CVS Exam:
Patient had AS
Q's
• Other causes of ESM --Hypertrophic cardiomyopathy
• How to investigate to see if fit for surgery- ECHO to look at EF and gradient across valve
• Any important considerations for anaesthesia? No epidural, cause hypotension which can be compensated in AS due to fixed output state
5. Hx and brief resp exam
Completely normal exam, history of long-standing panic disorders
Q's
• Would you pass this lady in pre-assessment for an elective cholecystectomy
• What are the ASA gradings? - what would she be?
• Can you think of ways to optomise her- SSRI trial
Anatomy (3):
1. Upper limb, prosection, live patient and skeleton all in one: Rapid fire 20 questions e.g- where is the insertion of supraspinator, (demonstrate on skeleton), demonstrate pronation and supination (live pt) point out long head of biceps (pro-section)
2. Unmanned prosection of mediastinum and thorax in saggital section. Lots of flags- just had to identify the structures - was v hard !
3. Manned station- very easy, lower GI/ Hepatobillary -prosection of bowels- asked blood supply, significance of water shed area and marginal artery of drummond. Also was given a colonoscopy picture of bowel ca and asked to identify it. Then asked dukes classification. Then hepatobillary anatomy on another prosection Skills
(2): Taking blood cultures Important points: patient was there- there were marks for interacting.
If you spoke to her, she told you she was IVDU and Hep +ve, so u had to take appropriate cautions-eye protection, and noting it on the form for the lab. Change needles before you fill bottles, and fill aerobic first. Offer to label them.
Also they had an obs chart and it said she was Pen allergic.
They said she had a new murmur, and was spiking on obs chart and asked for a differential. I said that I wld query infective endocarditis, they asked organism, I said staph, and they asked me if I want to write up Abx- I did, VANC--> she was penn allergic which was the trick of the station.
Scrubbing Self explanatory
Other stations:
Critical Care: Definitions of sepsis, septicaemia, septic shock etc. Asked for intepretation of a HDU chart, and generally where and how to ressucitate a patient in shock, ABCDE...
Comm skills- Calming an eratic mother whose son had been in accident in playground and was on the table for an emergency splenectomy. Had to tell her risk and complications, long term e.g immunizations. and she was questioning why he was taken to surgery without consent, so u had to to know the legislation that the doc act in interest of child if no consenting adult is available in an emergency Comm skills- Discharge summary.
Information Giving- Polytrauma patient, needed to read notes in prep station and call trauma surgeon at home who is on call. He just asked questions to see if you knew the ATLS guidelines, and about management of open fractures.
Information Receiving (written stations)
ECG: AF with fast ventricular response- asked to inteprate rate/ rhythm, about reversible causes, and treatment
CT- Bilateral pleural effusions in a pancreatitic- asked about ARDS, and glasgow scoring
Erect Chest X-Ray- Perforated viscus
Hope these are useful and good luck!
Clinical Skills and History Taking
1. Examine this ladies neck I started peripherally with a thyroid status exam, but the examiner prompted me to go directly to the neck. She was an afrocarribean lady with what I thought was bilateral parotid enlargement:
Q's
• Causes of symmetrical bilateral parotid enlargement
• What is most likely cause in her (sarcoidosis)
• He asked me about other manifestations outside the neck
2. Examine this lump on a man's back:
Large lipoma- I examined including assessing for fixity to muscle, transillumenence, draining lymph nodes etc
Q's
• What muscle was it overlying
• What is blood supply and lymph drainage of that muscle (was Lat Dorsi)
• To describe how you would excise this lipoma
• Consent patient for procedure
3. HISTORY:
Very simple history for likely colorectal Ca,
Q's
• RF for colorectal ca
• Difference in presentation for IBD and colorectal ca --> why is this change in bowel habit Crohns or UC
• How you would investigate him
• Why CT pneumocolon is inferior to colonoscopy (you can biopsy with latter)
4. CVS Exam:
Patient had AS
Q's
• Other causes of ESM --Hypertrophic cardiomyopathy
• How to investigate to see if fit for surgery- ECHO to look at EF and gradient across valve
• Any important considerations for anaesthesia? No epidural, cause hypotension which can be compensated in AS due to fixed output state
5. Hx and brief resp exam
Completely normal exam, history of long-standing panic disorders
Q's
• Would you pass this lady in pre-assessment for an elective cholecystectomy
• What are the ASA gradings? - what would she be?
• Can you think of ways to optomise her- SSRI trial
Anatomy (3):
1. Upper limb, prosection, live patient and skeleton all in one: Rapid fire 20 questions e.g- where is the insertion of supraspinator, (demonstrate on skeleton), demonstrate pronation and supination (live pt) point out long head of biceps (pro-section)
2. Unmanned prosection of mediastinum and thorax in saggital section. Lots of flags- just had to identify the structures - was v hard !
3. Manned station- very easy, lower GI/ Hepatobillary -prosection of bowels- asked blood supply, significance of water shed area and marginal artery of drummond. Also was given a colonoscopy picture of bowel ca and asked to identify it. Then asked dukes classification. Then hepatobillary anatomy on another prosection Skills
(2): Taking blood cultures Important points: patient was there- there were marks for interacting.
If you spoke to her, she told you she was IVDU and Hep +ve, so u had to take appropriate cautions-eye protection, and noting it on the form for the lab. Change needles before you fill bottles, and fill aerobic first. Offer to label them.
Also they had an obs chart and it said she was Pen allergic.
They said she had a new murmur, and was spiking on obs chart and asked for a differential. I said that I wld query infective endocarditis, they asked organism, I said staph, and they asked me if I want to write up Abx- I did, VANC--> she was penn allergic which was the trick of the station.
Scrubbing Self explanatory
Other stations:
Critical Care: Definitions of sepsis, septicaemia, septic shock etc. Asked for intepretation of a HDU chart, and generally where and how to ressucitate a patient in shock, ABCDE...
Comm skills- Calming an eratic mother whose son had been in accident in playground and was on the table for an emergency splenectomy. Had to tell her risk and complications, long term e.g immunizations. and she was questioning why he was taken to surgery without consent, so u had to to know the legislation that the doc act in interest of child if no consenting adult is available in an emergency Comm skills- Discharge summary.
Information Giving- Polytrauma patient, needed to read notes in prep station and call trauma surgeon at home who is on call. He just asked questions to see if you knew the ATLS guidelines, and about management of open fractures.
Information Receiving (written stations)
ECG: AF with fast ventricular response- asked to inteprate rate/ rhythm, about reversible causes, and treatment
CT- Bilateral pleural effusions in a pancreatitic- asked about ARDS, and glasgow scoring
Erect Chest X-Ray- Perforated viscus
Labels:
Anatomy,
Critical care,
exams,
MRCS,
Revise,
Royal college of surgeons
Subscribe to:
Comments (Atom)