a) The hard portfolio
b) The actual interview
The hard portfolio is a very important way to demonstrate all your skills, achievements and also your organisation. Its upto you whether you use a lever arch file with dividers or a book. Either way there are principles that you must follow and some tips to make your book look impressive:
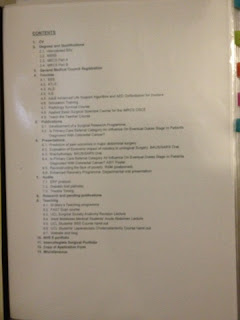
- Have a contents page and ensure dividers correspond with this
- Organise your book in logical sections
- Avoid bunching up lots of pages in one pocket, your portfolio should read like a book so that interviewers can quickly flick through
- Include a recent copy of your CV after the contents
- Ensure that you add any certificates for courses as well as your MBBS certificate etc...
- Don't forget your GMC certificate, copy of your application form and anything else they mention on the website
- Organise printouts from your e-portfolio into CEXs in one pocket, dops in one pocket etc with the most recent and flattering first! Also don't forget the minipats/msf print outs
- If you can print copies of presentations/posters in colour then please do to make them stand out
- Don't forget teaching achievements!!!
- If you have a record of the operations you have helped in/done so far that will also be impressive. As a non trainee you can register and use the Intercollegiate Surgical curriculum Portfolio "ISCP" (www.iscp.ac.uk). I recommend this as it shows that you are already familiar with the programme that they will use for all surgical training. It is also a very nice way to display your operative rcord (if you have one). Do not worry about absolute number of surgeries as they know that not everyone has had much exposure to surgery.
- Be comfortable and prepared to reply to any question on anything in your portfolio!!
I have included pictures of my portfolio below to give you an example of how you can set one out if you're not sure where to begin.
The next bit is the actual interview. There are many books to help you prepare, the one I recommend is "
Medical Interviews: a comprehensive guide to CT, ST and Registrar interview skills - Over 120 medical interview questions, techniques and NHS topics explained". It has lots of good examples and basically goes through how to structure answers to questions. Also, this WEBSITE has some good free content.
First of all, turn up looking smart and clean as well as early. Make sure you have brought your portfolio as well as all the necessary paperwork including photocopy of front cover of your passport, photo ID, passport pics etc... Try not have a smoke (or drink) before hand ;)
My interview (in 2011 for the London Deanery at Lions court) was split into three sections:
CLINICAL STATION:
please note. This is the most important station and weighted the most. I had two examiners and each gave me a scenario to answer.
- The first scenario was of an elderly woman post anterior resection 1 day ago. You are called to see her as she has a low urine output. It is important with this question to say you would firstly ensure that basic ALS principles are applied by ensuring patient was stable ie ABC... Then I said I would take a history and examine the patient to look for evidence of bleeding, infection, peritonism (think anastomotic leak) etc... Then look at the obs chart and look at trends for urine, fluid balance, BP, PR, temperature as well as latest bloods esp post-op. I would ensure patient is stable and let registrar and consultant know. You need to mention what possible differentials are going through your head and how you would exclude...
- The second Scenario was of a patient who rolled over in bed and came to A+E with a fractured humerus. BE ACREFUL AND LISTEN TO QUESTION AS I APPROACHED THIS AS A TRAUMA AS THOUGHT HE FELL BUT ITS NOT! Basically, on xray he ad luscent areas. You need to say you would suspect pathological fracture and screen for malignancy through history, exam and then can possibly send off tumour markers/myeloma screen etc... make sure you show them you know which tumours metastasise to bone and how you would check for them.
- Some of my friends got asked how they would manage a kid who came in with a supraconduylar fracture (must talk about risk of neurovascular compromise if displaced) as well as abdominal tenderness after falling off tree. In both these scenarios ATLS principles are important and ensuring you tell seniors early on (the latter point goes for everything)
MANAGEMENT STATION:
This station was a tad disorganised. I was again given two scenarios to talk through.
- The first was that one of my F1's tells me that he felt persecuted by the Consultant. You have to show that you would be understanding and caring toward your colleague but also resepctful of the right channels to pursue. You would ask them why they feel bullied. If its because they don't have enough knowledge maybe you could offer to tutor them etc. Otherwise you would encourage them to discuss with their supervisor/pastoral mentor to get advise. You would act in a supporting role. Whatever you do, don't say you would tell them to "man up" - it doesn't go down well no matter how tempting...
- The next was how would I ago about organising the rota - snooze fest! Basically you need to balance adequate training in terms of clinic, study leave, operating time with annual leave. I spent a lot of time talking about annual leave, THEY WERE NOT IMPRESSED!! Basically rota also needs to be EWTD compliant so other ways you can ensure people get adequate training is by using simulators etc...
PORTFOLIO STATION:
By far, this was the nicest station although it is less weighted than the others. I had a panel of 4 judges and they had looked through my portfolio before-hand (you hand it in before your other stations start) and asked questions about my teaching (including plans I had for developing this blog and website :)). I was also asked:
- What speciality I want to do and why? (I mentioned plastics and also let them know that I am aware how competitive it is by rattling off some statistics on past numbers etc)
- How will I develop my CV to increase my chances of getting a number in plastics?
- Other people where asked: what in their CV shows a dedication and commitment to medicine, teaching, why they chose that particular deanery...
Anyway, I hope some of this is useful and I will try and get some more info on his year's interviews to help next year's applicants. Good luck and remmebr to be confident, relaxed and know your porfolio/CV.